In the First of a Series of Articles, Natalie Heighway Examines the Process of Appointing First-Contact Physiotherapists to the Multidisciplinary Primary Care Team
| Read This Article to Learn More About: |
|---|
|
The Network Contract Directed Enhanced Service (DES) aimed for 100% geographical coverage by July 20191 as part of Investment and evolution: a five-year framework for GP contract reform to implement the NHS long term plan.2 Under the Network Contract DES, funding is available to primary care networks (PCNs) until 2024 through the Additional Roles Reimbursement Scheme (ARRS) to enable them recruit up to an additional 20,000 full-time equivalent (FTE) posts1 and develop a wider multidisciplinary team (MDT) in primary care. As of 31 December 2022, recruitment through the ARRS stood at 25,262 additional FTE posts, with funding available for a total of 26,000.3
On top of this additional funding, key changes to the GP contract in 2023–2024 added advanced clinical practitioner nurses to the reimbursable roles,3 and increased the cap on advanced practitioners from two to three whole-time equivalent (WTE) posts for PCNs with a list size of 99,999 or fewer and from three to six WTE posts for PCNs with a list size of 100,000 or more.3,4 In addition, the cap on mental health practitioners was removed.3 Since April 2023, PCNs have also been able to apply for reimbursement for the time that first-contact practitioners spend out of practice receiving education and training to become advanced practitioners.3
The maximum reimbursement amounts per role for 2023–2024 have also changed (see Tables 1 and 2).4 These amounts can be used to improve staff recruitment and retention, as wages can be increased in line with them; consequently, the core cost base of general practice is likely to increase beyond 2023–2024. Staff employed through the scheme will also be considered part of the core general practice cost base after 2023–2024, so use of permanent contracts is encouraged.3
Table 1: Maximum Reimbursement Amounts per ARRS Role for 2023–2024 (1 July 2023–31 March 2024)4
| Indicative band | Annual equivalent maximum reimbursable amount per role | Annual equivalent maximum reimbursable amount per role plus inner HCAS | Annual maximum reimbursable amount per role plus outer HCAS | |
| National | Inner London | Outer London | ||
| Clinical pharmacists | 7–8a | £62,340 | £72,269 | £69,308 |
| Pharmacy technicians | 5 | £40,159 | £48,442 | £46,371 |
| Social prescribing link worker | Up to 5 | £40,159 | £48,442 | £46,371 |
| Health and wellbeing coaches | Up to 5 | £40,159 | £48,442 | £46,371 |
| Care co-ordinators | 4 | £33,396 | £40,326 | £38,924 |
| Physician associates | 7 | £60,401 | £70,330 | £67,369 |
| First contact physiotherapists | 7–8a | £62,340 | £72,269 | £69,308 |
| Dietitians | 7 | £60,401 | £70,330 | £67,369 |
| Podiatrists | 7 | £60,401 | £70,330 | £67,369 |
| Occupational therapists | 7 | £60,401 | £70,330 | £67,369 |
| Nurse Training Associates | 3 | £29,649 | £36,227 | £35,177 |
| Nursing Associates | 4 | £33,396 | £40,326 | £38,924 |
| Community Paramedics | 7 | £60,401 | £70,330 | £67,369 |
| Advanced Practitioners | 8a | £68,315 | £78,243 | £75,282 |
| General Practice Assistant | 4 | £33,396 | £40,326 | £38,924 |
| Digital Transformation Lead | 8a | £68,315 | £78,243 | £75,282 |
| Apprentice Physician Associate | 5 | £40,159 | £48,442 | £46,371 |
| ARRS=Additional Roles Reimbursement Scheme; HCAS=high cost area supplement NHS England. Network Contract DES contract specification 2023/24—PCN requirements and entitlements. London: NHS England, 2023. Available at: www.england.nhs.uk/wp-content/uploads/2023/03/PRN00157-ncdes-updated-contract-specification-23-24-pcn-requirements-and-entitlements-updated.pdf Contains public sector information licensed under the Open Government Licence v3.0. | ||||
Table 2: Maximum Reimbursement Amounts for Mental Health Practitioners for 2023–2024 (1 July 2023–31 March 2024)4
| AfC Band | Annual equivalent maximum reimbursable amount per role | Annual equivalent maximum reimbursable amount per role plus inner HCAS | Annual equivalent maximum reimbursable amount per role plus outer HCAS | |
| Adult Mental Health Practitioner and CYP Mental Health Practitioner | 4 | £16,698 | £20,163 | £19,462 |
| 5 | £20,080 | £24,221 | £23,186 | |
| 6 | £24,760 | £29,724 | £28,244 | |
| 7 | £30,201 | £35,165 | £33,684 | |
| 8a | £34,157 | £39,122 | £37,641 | |
| CYP=children and young people; AfC=Agenda for Change; HCAS=high cost area supplement NHS England. Network Contract DES contract specification 2023/24—PCN requirements and entitlements. London: NHS England, 2023. Available at: www.england.nhs.uk/wp-content/uploads/2023/03/PRN00157-ncdes-updated-contract-specification-23-24-pcn-requirements-and-entitlements-updated.pdf Contains public sector information licensed under the Open Government Licence v3.0. | ||||
During 2023–2024, NHS England will review the ARRS to ensure that it is fit to deliver future ambitions for general practice. However, education and training of both the primary care team and ARRS staff is necessary for additional roles to reach their full potential. Using the Shropshire, Telford and Wrekin (STW) Integrated Care System (ICS) as a case study, this series of articles examines the process of recruiting and embedding first-contact physiotherapists (FCPs)—one of the 18 additional roles currently appointable through the ARRS4—into the primary care MDT, and how practices can best harness the benefits of practice-based physiotherapists.
First-Contact Physiotherapists in the STW ICS
First-contact physiotherapists are designed to support GPs as part of the integrated care team and to optimise the care pathway by ensuring that patients see the right person, in the right place, first time.5 A first-contact practitioner is a diagnostic clinician working at the top of their clinical scope of practice at Master’s level, allowing them to assess and manage undifferentiated and undiagnosed musculoskeletal (MSK) presentations.5
Within the STW ICS, 26 FCPs are currently employed using four different models:
- employment by a PCN
- employment by a private provider
- employment by two different NHS trusts.
Although the FCPs in STW are employed using different models, they are embedded in the PCN’s core network practices.4 Most work out of multiple practices in their PCN, which allows them access to other healthcare professionals and all electronic ‘live’ and paper-based record systems, as stated in the additional role requirements.4 They receive support from duty clinicians in the practices, and also from their employer and the wider system through the FCP Facilitator and author of this article, Natalie Heighway.
In addition, FCPs in STW have access to a variety of types of clinical supervision, which is also a requirement for ARRS staff.4 The clinical supervision and support provided will be discussed in more detail in article two of this series.
ARRS Workforce Planning and Redistribution of Funding
The Network Contract DES required PCNs to complete and return to the Commissioner a workforce plan, using the agreed national workforce planning template, by 31 August 2023.4 This allows commissioners to review expenditure and assess any ‘unclaimed funding’, which other PCNs can then ‘bid’ for.4 The way this will work can be expected to differ between ICSs; in STW, workforce plans will likely use all of the available funding if roles are filled (source: internal data from STW ICS). The Commissioner is responsible for giving other PCNs the opportunity to bid for unclaimed funding, explaining how and when to do this, and notifying PCNs of the outcome.4
The Commissioner must then explore different ways of supporting the PCN to implement the workforce plan.4 In STW, for example, the following are underway:
- the FCP Facilitator is investigating ways to support recruitment through involvement with job descriptions, applications, and interviews
- the Commissioner is exploring new ways of working and recruitment as part of the Musculoskeletal Transformation Team, with the aim of supporting primary care
- the provision of rotational working is being looked into for FCPs across acute and community providers working with the new Musculoskeletal Services Shropshire and Telford6
- career pathways are being devised for physiotherapists (including FCPs) to link NHS workforce plans for the local system with PCNs’ workforce plans.
ARRS Minimum Role Requirements
Each additional role has its own minimum requirements, set out in Annex B of the Network Contract DES.4 These requirements will now be discussed using FCPs in STW as an example.FCPs need to comply with Health Education England’s First contact practitioners and advanced practitioners in primary care: (musculoskeletal) a roadmap to practice,5 which reflects the requirements set out in Annex B of the Network Contract DES.4 FCPs need to be experienced: they are required to assess, diagnose, and manage undifferentiated MSK presentations,5 and rule out non-MSK presentations. Figure 1 illustrates the process of a physiotherapist becoming an FCP.5
Figure 1: Career Progression of Primary Care Roles5
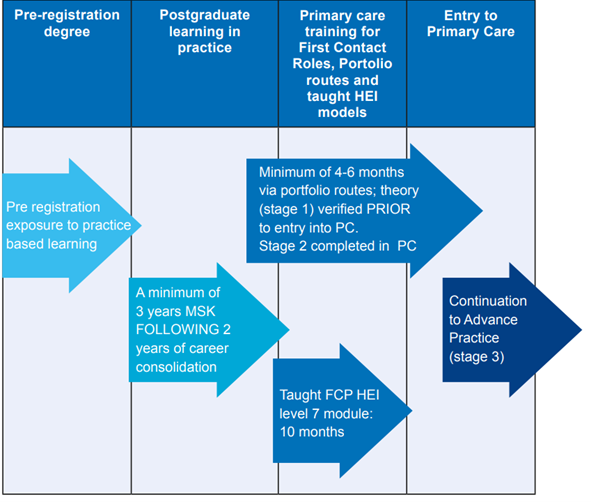
Health Education England. First contact practitioners and advanced practitioners in primary care: (musculoskeletal) a roadmap to practice. Leeds: Health Education England, 2021. www.hee.nhs.uk/sites/default/files/documents/MSK%20July21-FILLABLE%20Final%20Aug%202021_2.pdf
Contains public sector information licensed under the Open Government Licence v3.0.
Verification
The FCP roadmap verification process has recently changed:7 from April 2024, FCPs will need to complete the process through a university. This may be via taught Master’s modules funded by NHS England, or via a portfolio route and signed off by a registered university. There will no longer be a register of verified FCPs or ‘digital badge’ allowing FCPs to display their credentials. Instead, portfolio paperwork completed before April 2024—or a university certificate obtained before or after April 2024—will be evidence of successful completion of both stages 1 and 2 of the FCP roadmap.7
Accountability
The Care Quality Commission (CQC) states that providers are accountable for staff who they may not employ directly, but who deliver regulated activity on their behalf.8 Providers must therefore make sure that staff are competent.8 This assurance can be gained from confirming that FCPs have completed the roadmap and are working at the level required for primary care first-contact roles. Stage 1 of the FCP roadmap should be completed before employment in primary care, and stage 2 should be completed when working in primary care. This should be within 6 months for those in FTE FCP roles, or longer if the provider and Commissioner agree.8
It is important to note that the CQC will expect to see evidence or assurance that staff recruited to FCP roles have completed stage 1 of the roadmap. It will also expect to see arrangements for completion of stage 2 of the roadmap.8
Recruitment Checks and Supervision
Providers also need to ensure that the staff they manage have the appropriate recruitment checks, professional registration, and supervision, irrespective of who holds the employment contract.8 In STW, this process is different for each employment model: in our experience, with private providers, assurance is obtained through the use of letters of confirmation that a clinical supervisor is assigned to each FCP; NHS trusts hold service-level agreements with PCNs that include details regarding supervision; and FCPs employed directly have supervision in their contracts in most PCNs.
Shropshire, Telford and Wrekin Primary Care Workforce and Training Hub also offers financial and organisational support with clinical supervision to PCNs and practices, allowing FCPs to receive direct clinical supervision in their place of work with the aim of improving integration, shared learning, recruitment, and retention. In our organisation, day-to-day clinical supervision is also provided by the duty GP for all clinical staff.
If FCPs are appropriately qualified for the roles and have the necessary supervision, they will have no problem meeting the key responsibilities outlined in the Network Contract DES.4 FCPs in STW work independently with a patient list, assessing, diagnosing, triaging, and managing patients in primary care, and referring patients on to the wider MSK pathway when necessary.5 They support the wider MDT, offering second opinions on patients and answering questions from other clinicians, as they are the specialist on MSK conditions in general practice.5
Additional Training and Development
When managing patients in primary care, FCPs offer tailored care when appropriate and within their scope of practice, including:4
- personalised exercise programmes and education
- injections
- independent prescribing.
FCPs who wish to use therapeutic injection therapy as part of their practice need to complete education and training that meets Chartered Society of Physiotherapy expectations, including 150 hours of training with supervised practice and a formal assessment of capabilities, which is usually through a university Master’s module.9
FCPs who have completed a validated and approved prescribing module by the Health and Care Professions Council (HCPC) and have their prescribing qualification added to their HCPC registration can prescribe.9 FCPs who are appropriately qualified can perform supplementary or independent prescribing.4,10 Supplementary prescribing is the use of a written clinical management plan (CMP) to prescribe agreed medicines in partnership with a doctor. The CMP can include any licensed or unlicensed medicines and certain controlled drugs.10 Independent prescribers may prescribe any licensed medicine from the British National Formulary, within national and local guidelines, for any condition within their area of competence;10 in primary care, FCPs who are independent prescribers take responsibility for making and justifying these treatment decisions.4
Where the local ICS permits, FCPs can also request investigations.4 This is currently not permitted in STW, but it is being explored for its potential to improve patient care, evidence-based practice, and access to services.
The wider responsibilities of FCPs include providing leadership and support on MSK clinical and service development across the PCN and learning opportunities for the MDT in primary care, encouraging collaborative working across the wider health economy, and supporting regional and national research and audit programmes to evaluate and improve the FCP programme.4
Summary
The ARRS offers primary care the opportunity to widen the expertise of the MDT through the appointment of additional roles such as FCPs. However, unless FCP services are set up, clinical and nonclinical practice staff and the public are educated about the capabilities of FCPs, and—most importantly—the right people are employed and given adequate supervision and training, FCPs will be unable to meet their primary aims of seeing the right patients first time, increasing capacity and appointments in primary care, and reducing the workload of GPs.
| The second article in this series will explore the support offered to FCPs and general practice by the Shropshire, Telford and Wrekin Primary Care Training Hub, highlighting key learning points and development opportunities. |


