Dementia: comorbidities in patients - data briefing
Published 1 November 2019
1. Purpose
This briefing shows findings from the analysis of a sample of anonymised primary care records in relation to the prevalence of diagnosed comorbid conditions of patients with a diagnosis of dementia.
The target audiences for this briefing are health commissioners and providers of primary care and community services supporting patients with dementia. These findings are available and presented at a national level with the intention that they are then interpreted to inform a local assessment of the needs of patients with dementia and the provision of health and care services.
2. Main findings
A total of 77% of patients with dementia also have at least one of the specific health conditions considered in this study. This compares to 68% in the all patient group for the same list of health conditions (excluding dementia).
For patients with dementia, 44% have a diagnosis of hypertension, between 17% and 20% have a diagnosis of diabetes, stroke or TIA, CHD or depression, while between 9% and 11% have a diagnosis of Parkinsonism, chronic obstructive pulmonary disease or asthma.
The prevalence rate for 8 of the 10 specific health conditions is higher for patients with dementia when compared to the all patient group. The prevalence rates for hypertension and asthma are lower than the all patient group.
Patients with dementia are more likely to have multiple health conditions. A total of 22% with 3 or more comorbidities and 8% with 4 or more comorbidities, compared to 11% and 3% respectively in the all patient group.
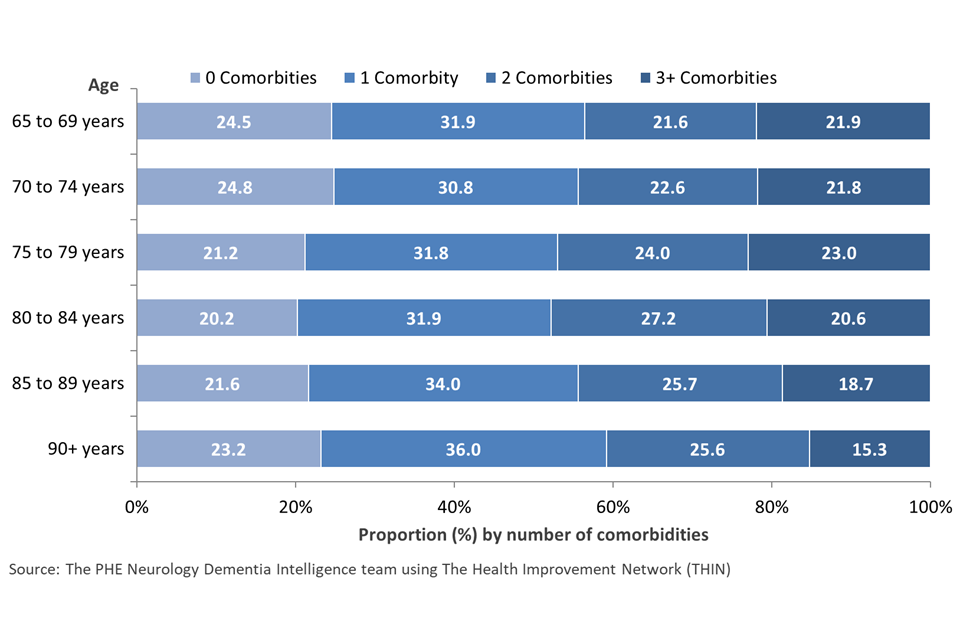
The proportion of patients aged 85 years and older with 2 or more other health conditions recorded in the primary care notes is lower than the proportion in age groups under 85 years. Diagnosing comorbidities in patients with dementia can be more difficult to achieve as the severity of dementia increases. However, it can lead to comorbid conditions being under-diagnosed and thus health needs of patients remaining unmet.
3. Background
The number of people living with dementia in the UK is estimated to be around 850,000 and set to increase, with figures anticipated to reach over one million by 2025 [footnote 1].
The All Party Parliamentary group (APPG) report from 2016 [footnote 2] suggested almost 7 in 10 people with dementia also have one or more other health condition.
These health conditions, known as comorbidities, include:
- hypertension (high blood pressure)
- depression
- coronary heart disease (CHD)
- stroke or transient ischaemic attack (stroke or TIA)
- diabetes
The APPG asked that Public Health England (PHE) “do more to provide health and social care commissioners with data on dementia and common comorbidities”.
This study supplements the APPG qualitative investigation [footnote 2], by providing an analysis of a large sample of primary care records using The Health Improvement Network (THIN) [footnote 3] dataset. The study investigates 10 specific physical health, mental health and neurological comorbid conditions and compares their rate of prevalence with the all patient group in the dataset. It asks:
- are patients with dementia more likely to also have other health conditions than the all patient group?
- are patients with dementia more likely to have multiple health conditions than the all patient group?
- is there any difference in comorbidity patterns for different types of dementia?
4. Methodology
4.1 Defining the cohort for the study
The study cohort (patients with dementia) are those patients who have primary care records in THIN dataset, aged 65 years and older and that have a diagnosis for the following forms of dementia recorded (including International Classification of Diseases ICD 2010 codes [footnote 4]):
- Alzheimer’s disease (F00 & G30)
- vascular dementia (F01)
- dementia in other diseases (F02) such as Parkinson’s disease or Pick disease [footnote 5]
- other degenerative diseases of the nervous system (G31)
- unspecified dementia (F03)
Primary care record systems use Read codes [footnote 6] to record patient activity. The list of ICD 10 codes above was mapped to the equivalent Read codes using cross mapping files [footnote 7] and reviewed by clinicians to ensure appropriateness of approach.
The comparator group for this study is the all patient group who have primary care records in the THIN dataset, aged 65 years and older. The all patient group includes the patients with dementia.
The term ‘patients with dementia’ is used throughout this briefing as the analysis is of activity of people with dementia associated with health care provision.
4.2 Health conditions included in this study
The APPG report identifies 5 conditions that people with dementia commonly live with that can increase the risk of developing dementia (hypertension, CHD and diabetes) and are associated with dementia (stroke or TIA, depression).
This study includes additional neurological conditions (Parkinsonism and epilepsy) and mental health conditions - severe mental illness or psychosis (SMI) - that have a known association with dementia [footnote 5],[footnote 8]. Respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD) are also part of the study as general physical health comparators.
For all the above conditions, except for Parkinsonism, definitions are available from the Quality and Outcomes Framework (QOF) business rules [footnote 10]. The epilepsy definition has been amended to include all those with a recorded diagnosis of epilepsy regardless of current treatment status. The definition of Parkinsonism uses a list of ICD10 codes published by PHEs Neurology Intelligence Network (NIN)[footnote 11] and then mapped to Read codes.
4.3 Dataset used in this study
The dataset used in this study is The Health Improvement Network (THIN)[footnote 3] and is a UK primary care electronic medical record data resource covering around 375 GP practices and just under 3 million active patients. The coverage for England is around 2% of practices and 2% of registered patients.
The dataset is based on extracts from GP systems that are taken every 4 months. Each extract is known as a new version of THIN. This analysis is based on data extracted during August 2016. The dataset contains anonymised records for 536,738 patients aged 65 years and older of which 21,917 have a diagnosis of dementia. The prevalence rate for dementia in the THIN dataset is between 4% and 4.1%. The prevalence rate in the England population is 4.3% for the comparable period [footnote 12].
4.4 Limitations of the study
This study was focussed on the analysis and interpretation of the sample primary care dataset (THIN). A limited literature review was undertaken to identify health conditions that would be considered relevant to people with dementia and could be validated using existing published data sources such as the Quality and Outcomes Framework (QOF) [footnote 12].
The process for the selection of comorbidities considered in this study was informed by the APPG report, conditions managed in primary care and the availability of data and definitions published through QOF. Some physical health conditions have been excluded from analysis. These conditions can be responsible for hospital admissions for older people and include falls, fractures, or chronic pain. Cancer related health conditions were also excluded .
The findings in this study are dependent on how data on patient activity is recorded on primary care systems. One issue is the use of the term ‘unspecified dementia’. This classification is not included in reference material produced by Alzheimer’s society [footnote 9], but is a common occurrence in operational datasets, when insufficient detail is recorded in communication exchanges between practitioners. The consequence of this is that by dementia subtype, the proportions found in this study may differ from other published sources.
A second issue relates to quality of diagnosis. It is not always possible to determine the true diagnosis of dementia or dementias for an individual without an autopsy of brain tissue. Other sources have indicated that mixed dementias are more common for those in older age groups [footnote 9].
In section 4.4 of this briefing, the representative nature of THIN dataset compared to the England registered patient population in terms of age and sex is discussed. However, no assessment has been made in relation to the ethnicity of patients or the level of social deprivation in which the patient resides.
4.5 Presentation of findings
Data presented in figures 1 to 4 and 6 have been age and sex directly standardised using the European Standard Population [footnote 13]. Data presented in figures 5 and 7 related to proportion aggregated from the data source.
The prevalence rates are calculated using the standardised counts of those with a diagnosis of a specific condition recorded in the data source for both the patients with dementia and the all patient group and then divided by the corresponding standardised cohort count.
Difference in the calculated statistics is determined by use of 95% confidence intervals (CI). For this study, a statistic is considered significantly different from its comparator if the corresponding CIs are not overlapping.
5. Findings
The THIN dataset contains anonymised records for 21,917 patients aged 65 years and older who have a diagnosis of some form of dementia. In the patient with dementia group, 65% are female and 35% are males, 88% are aged 75 years and older and 12% are between 65 years and 74 years of age. Females aged 85 years and older account for 34% of the dementia group.
A diagnosis of Alzheimer’s disease accounts for 38% of those patients with dementia, with 25% having a diagnosis of vascular dementia, 3% have mixed dementias, while 29% of the cohort have an unspecified type of dementia recorded in the primary care record.
5.1 Patients with dementia and other health conditions
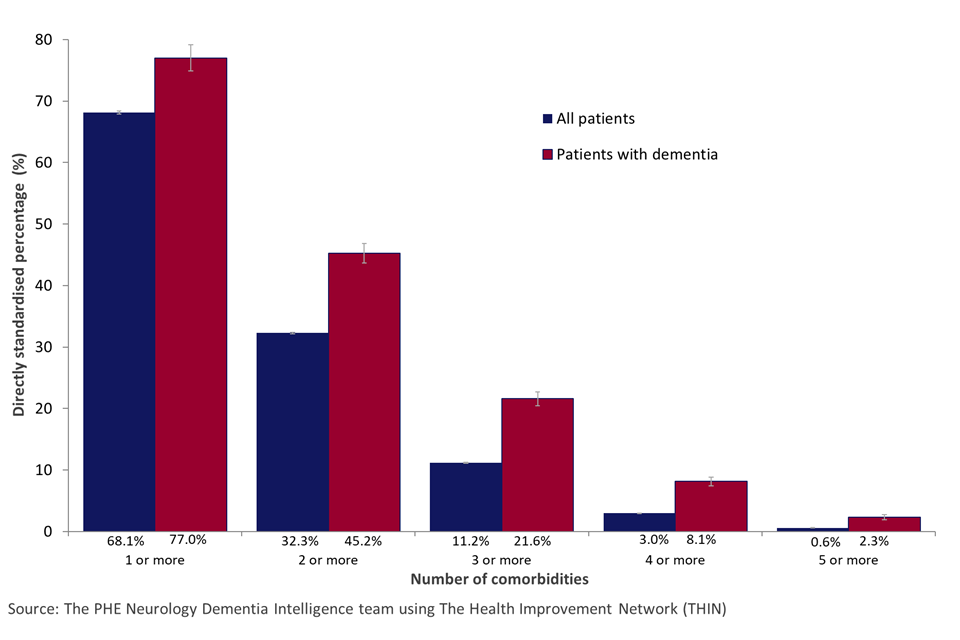
In this study 77% of patients with dementia also have a diagnosis recorded for one or more other specific comorbidity. This compares with 68% in the all patient group, for the same list of health conditions (Figure 1). A total of 23% of patients with dementia have no other comorbidity recorded in the primary care notes.
As the number of comorbidities recorded increases, Figure 1 shows that the proportion of patients in both the dementia group and the all patient group decrease. However, the proportion of patients with dementia remains higher than the all patient group, with the difference in the proportion increasing as the number of comorbidities increases. 22% of patients with dementia have 3 or more comorbidities and 8% have 4 or more, compared to 11% and 3% respectively in the all patient group.
Figure 1: Percentage of patients by number of comorbidities (August 2016, directly age and sex standardised percentage registered patients, ages 65 years and older)
Prevalence of comorbid conditions
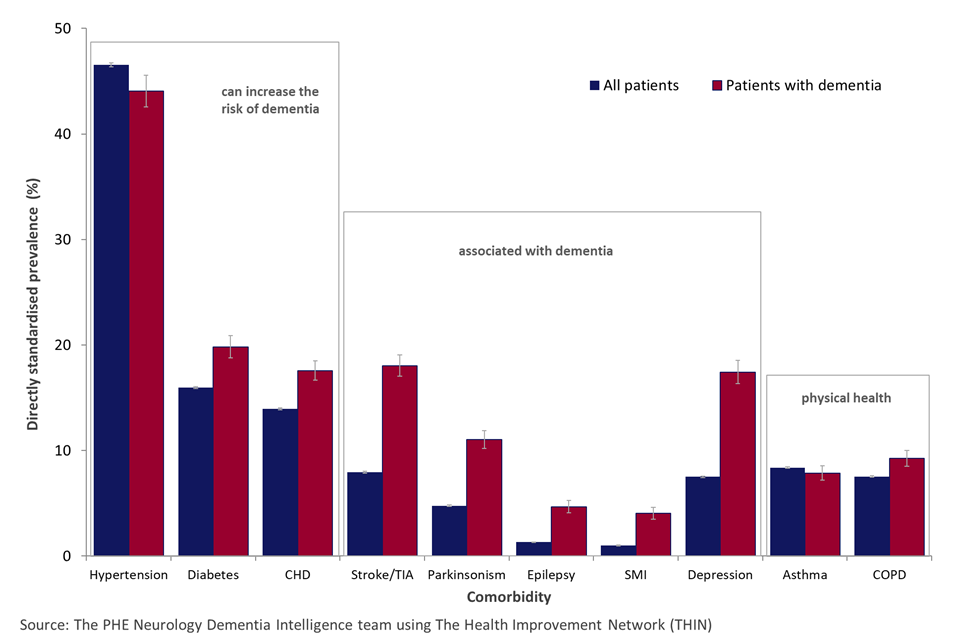
This study shows that the prevalence rates for the individual specific health conditions are generally higher among patients with dementia than the all patient group in the THIN dataset (Figure 2).
Hypertension (44%) is the most prevalent condition for patients with dementia, which is more than twice as common as diagnoses for diabetes (20%), stroke/TIA (18%), CHD (18%) and depression (17%). 11% have a diagnosis of Parkinsonism, 5% have epilepsy and 4% have SMI.
Although hypertension is the most common comorbidity for patients with dementia, the age standardised rate is greater in the all patients group (44% versus 47%). The rates for stroke/TIA (18% versus 8%), Parkinsonism (11% versus 5%), epilepsy (5% versus 1%), SMI (4% versus 1%) and depression (17% versus 8%) are all more than double in patients with dementia than in the all patient group. Patients with dementia are also more likely to have COPD (9%) than the all patient group (8%).
Figure 2: Condition prevalence for patients with dementia and all patients (August 2016, directly age standardised percentage, ages 65 years and older)
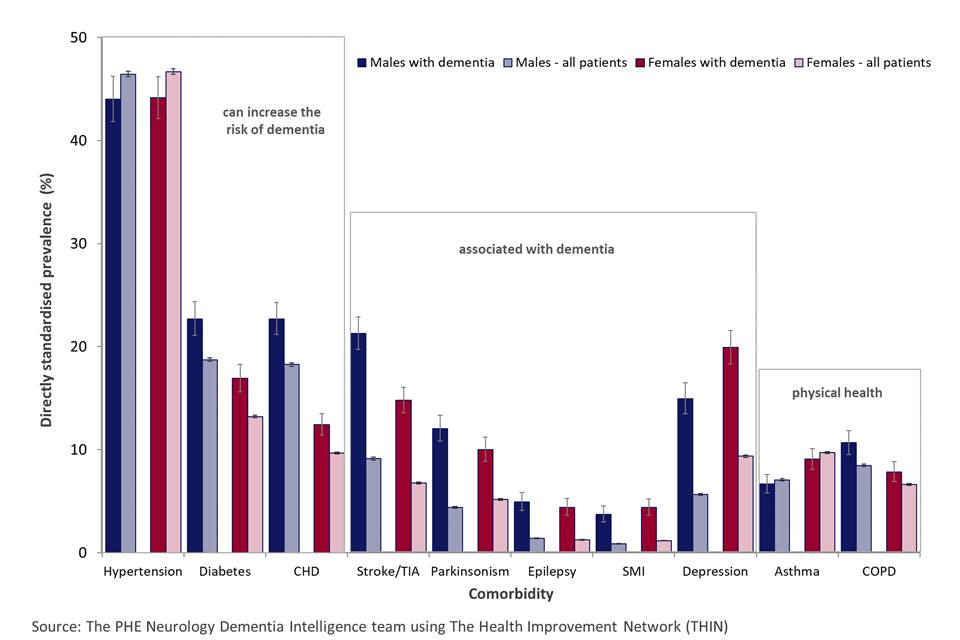
Comorbid conditions and sex of patient
The study found that for conditions that can increase the risk of dementia, the prevalence rates for CHD and diabetes are higher in males with dementia than females with dementia. Both groups being higher than the corresponding all patient groups (Figure 3). However, for rates of hypertension, there is no difference between males and females with dementia, and there is no difference between the 2 male groups. The prevalence of hypertension of females with dementia is lower than that of the all patient group.
For conditions associated with dementia, the prevalence rate of stroke or TIA in males with dementia is higher than in females with dementia (21% versus 15%). The prevalence for both groups being higher than the respective all patient group (9% versus 7%). For all other conditions in this group there was no difference between the rates for males and females and the dementia groups have higher rates than their respective all patient groups.
Females with dementia have a higher prevalence of depression than that of males with dementia (20% versus 15%), with again the 2 groups having higher rates than their respective all patient groups (9% and 6% respectively).
Asthma is more common in females with dementia than males with dementia (9% versus 7%). Males with dementia have a higher prevalence of COPD than females (11% versus 8%), again with both groups being higher than their respective all patient group (8% and 7% respectively).
Figure 3: Condition prevalence for patients with dementia and all patients by sex (August 2016, directly age standardised percentage registered patients, ages 65 years and older)
Comorbid conditions and age of patient
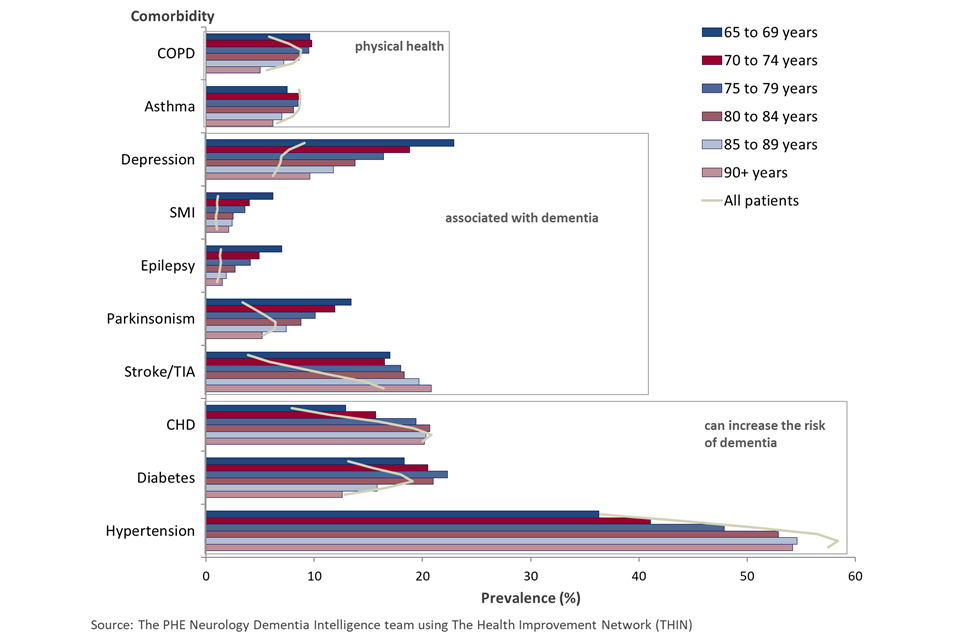
Figure 4 below shows that the pattern in prevalence rates of comorbidities across age bands varies considerably for each condition investigated in the study.
For the comorbidities that can increase the risk of dementia, the prevalence rates peak before the oldest age group. For hypertension the rates peak in the age band of 85 to 89 years, at 55%. For CHD the peak age is 80 to 84 years with a rate of 21% and for diabetes the peak rate of 22% is in the 75 to 79 years band. The rate distribution across age bands for patients with dementia is very similar to the all patient group.
With the comorbidities associated with dementia, there are 2 very different patterns associated with age. The prevalence of stroke or TIA increases with age, although the increase varies less in patients with dementia than the all patient group, due to higher rates in the dementia group.
The pattern in prevalence rates by age for Parkinsonism, epilepsy and SMI in patients with dementia decreases with age. The pattern for the all patient group is different. For epilepsy and SMI the prevalence rate across all ages remains constant, while for Parkinsonism the prevalence rate peaks at 80 to 84 years.
There is a decreasing pattern of prevalence rates across age groups for depression in patients with dementia which is similar to the pattern for the all patient group.
For COPD the prevalence in patients with dementia aged the under 80 years is fairly constant and then decreases by age. The pattern in the all patient group is different as it increases to a peak in the 75 to 79 years age band and then decreases with age.
Figure 4: Condition prevalence for patients with dementia by age (August 2016, directly age standardised percentage registered patients, ages 65 years and older)
5.2 Patients with dementia and multi morbidity
Figure 1 above shows that 77% of patients with dementia also have a diagnosis for at least one of the comorbidities included in the study. Furthermore, it shows that 22% have 3 or more comorbidities and 2% are living with 5 or more comorbidities considered in the study.
Figure 5 shows the number of comorbidities that patients with dementia are also diagnosed with by age band. Overall, 23% of patients in the dementia group do not have any other health condition considered in this study. By age group, the largest proportion of patients with no other health condition, are aged under 74 years of age, with the proportion decreasing to 20% for the 80 to 84 year olds. The proportions in the older 2 age groups increase again, with 23% of the 90 years and older having no other recorded comorbid condition.
Conversely, the proportion of patients in the dementia group with 3 or more comorbidities increases with age to 23% for the 75 to 79 year olds, but then decreases for the older groups to 15% for those aged 90 years and older.
The figure below also shows that the proportions of patients with dementia with 2 or more comorbidities increases with age for those aged under 85 years of age. However, the proportion decreases with age for those aged 85 years and older.
Figure 5: Proportion of patients with dementia (ages 65 years and older) with a number of comorbidities in addition to their dementia by 5-year age band (August 2016)
5.3 Comorbidities and different types of dementia
There are many different causes and types of dementia. Primary dementias include: dementia due to Alzheimer’s disease, vascular dementia, dementia with Lewy bodies and frontotemporal dementia (9). Alzheimer’s disease is the most common, followed by vascular dementia and dementia with Lewy bodies. Mixed dementia with features of more than one type, is now considered to be the commonest type of dementia, especially in older adults [footnote 9].
This section looks at the difference in comorbidities by type of dementia diagnosis. In this analysis patient dementia type has been determined by the most recent diagnosis code on their patient record.
As stated earlier, in this study 38% of the patients with dementia have a recorded diagnosis of Alzheimer’s disease, 25% have a diagnosis of vascular dementia, 3% have mixed dementias, while 29% of the cohort have an unspecified type of dementia recorded in the primary care record.
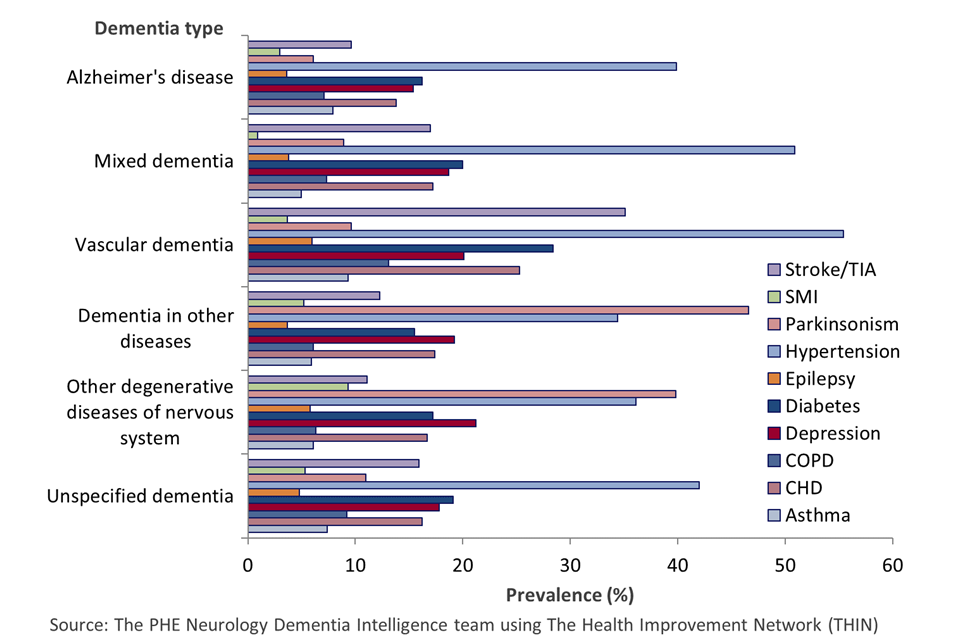
Figure 6 shows the comorbidity prevalence rates by dementia type. Overall patients with any type of dementia have high prevalence rates of hypertension, with rates ranging from 34% in those with dementia in other diseases, to 55% in those with vascular dementia. Parkinsonism is most common in patients with dementia in other diseases and other degenerative disease category.
A diagnosis of stroke or TIA is at least twice as likely in patients with vascular dementia (35%) than in all other forms of dementia. Diagnoses for depression are equally likely in all forms of dementia (15% to 21%), similar to the prevalence for diabetes (16% to 20%), except in vascular dementia where the prevalence rate is 28%.
Figure 6: Condition prevalence by dementia type (August 2016, directly age sex standardised percentage, ages 65 years and older)
5.4 THIN dataset
This study used the THIN dataset to investigate the issues raised by the APPG. This dataset was chosen because it is a sample dataset of primary care records that the Dementia Intelligence team at PHE currently have access to.
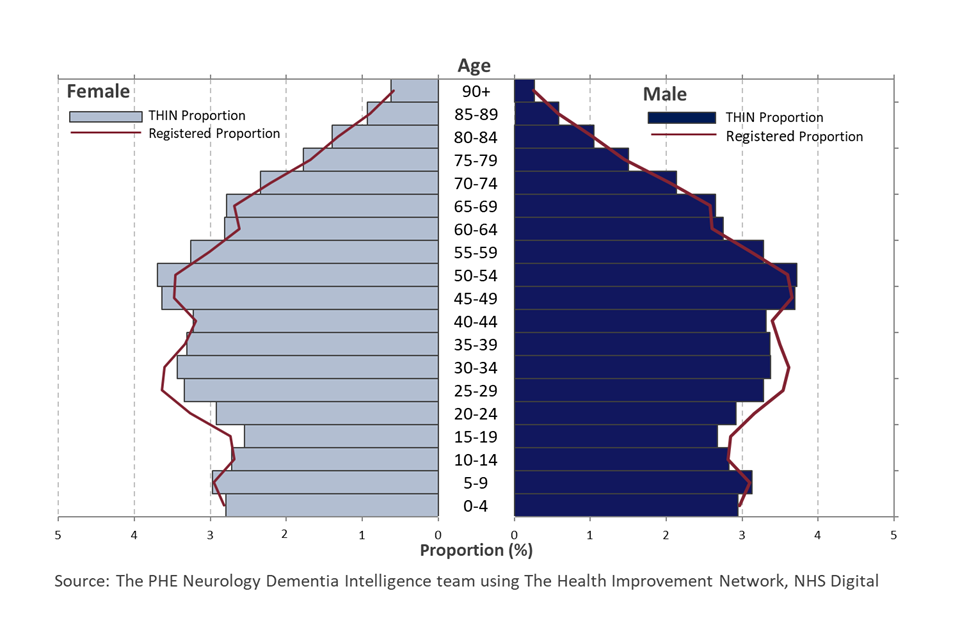
The THIN dataset contained anonymised records for 536,738 individuals aged 65 years and older. The demographic characteristics of the dataset are very similar when compared to registered populations in England. Patients in age groups 15 to 19 and 35 to 39 are slightly under represented in THIN, whereas those age groups between 45 years to 69 years are slightly over represented. This is more noticeable amongst females. The proportions of the population in each of the age sex groups for patients over 70 are almost identical in both sources. This is important for this work as this group make up the bulk of the population with a recorded dementia diagnosis.
Figure 7: Demographic distribution of THIN and registered patient list by age and sex (August 2016 (THIN), October 2016 (England))
Condition prevalence in THIN and England overall
Table 1 below includes the health conditions of interest in this study with the calculated rates and confidence intervals from the THIN dataset. Also included are the corresponding rates and confidence intervals for England, published through the QOF for comparison.
For 5 of the study comorbidities the rates calculated from the THIN dataset are above the corresponding QOF values and for 5 other conditions, they are below the rate. For all conditions except asthma, depression and epilepsy, the THIN calculated rates are very similar to the QOF. For the remaining 3 conditions, the THIN rates are around 1.5 times larger.
Epilepsy prevalence is higher in the THIN dataset because this analysis includes all those with a diagnosis, while QOF figures include only those currently on medication. The prevalence of both asthma and depression are also higher in the THIN dataset because both conditions can be marked as resolved within the records. In QOF a patient with a resolved code entered on their record later than a diagnosis code would no longer be considered to have the condition, whereas in this THIN analysis, they are included.
Table 1: Adult condition prevalence (per 100 patients/cases) in THIN and England registered population
| Condition (ages included) | THIN Prevalence (95% CI) | England Prevalence (QOF) (95% CI) |
|---|---|---|
| Dementia (65+) | 4.1 (4.0 to 4.1) | 4.3 (4.3 to 4.3) |
| Asthma (all ages) | 9.3 (9.3 to 9.3) | 5.9 (5.9 to 5.9) |
| CHD (all ages) | 3.1 (3.1 to 3.2) | 3.2 (3.2 to 3.2) |
| COPD (all ages) | 1.9 (1.9 to 1.9) | 1.9 (1.9 to 1.9) |
| Depression (18+) | 11.3 (11.2 to 11.3) | 8.3 (8.3 to 8.3) |
| Diabetes (17+) | 6.3 (6.3 to 6.4) | 6.6 (6.5 to 6.) |
| Epilepsy (18+) | 1.3 (1.2 to 1.3) | 0.8 (0.8 to 0.8) |
| Hypertension (all ages) | 13.4 (13.4 to 13.5) | 13.8 (13.8 to 13.8) |
| Parkinsonism (all ages) | 2.0 (1.9 to 2.0) | - |
| SMI (all ages) | 0.8 (0.8 to 0.8) | 0.9 (0.9 to 0.9) |
| Stroke/TIA (all ages) | 1.8 (1.8 to 1.8) | 1.7 (1.7 to 1.7) |
Source: The Health Improvement Network (THIN), NHS Digital
6. Conclusions
6.1 Patients with dementia and comorbidities
The findings of this study support the APPG conclusion that a large proportion of patients with dementia live with other health conditions. This study suggests that the proportion is close to 8 in 10, rather than the 7 in 10 quoted in the APPG report. The proportion of patients with dementia that have other health conditions (77%) is larger than the all patient group (68%).
The health conditions investigated in this study are dementia specific comorbidities categorised into 2 groups. Comorbidities that can increase the risk of dementia (hypertension, coronary heart disease, diabetes) and those that are associated with dementia (stroke or TIA, Parkinson’s disease, epilepsy, depression and SMI). This study found that hypertension was the most common other comorbidity that patients with dementia have a diagnosis for (44%). However, hypertension has a higher prevalence in the all patient group. For the 7 remaining health conditions the prevalence in patients with dementia is higher than the all patient group.
This study found that the proportions of patients with dementia and a diagnosis of SMI, depression, Parkinsonism or epilepsy decreases as age increases. However, there are increases in the proportions identified with hypertension, CHD and stroke or TIA, as age increases.
For the 2 physical conditions (respiratory conditions) considered in the study it was found that patients with dementia have a higher prevalence of COPD. The rate is no different for asthma. If consideration were to be made of other physical health conditions and cancers that affect the general ageing population, then the true figure for the proportion of patients with dementia living with other health conditions will likely be much higher.
Therefore, in conclusion, the findings of this study support the view that patients with dementia are more likely to have a diagnosis for other health conditions, as considered in this study, when compared with the all patient group.
6.2 Patients with dementia and multi morbidity
The findings of this study show that patients with dementia are more likely to have multiple health conditions and thus more likely to have complex health needs when compared to the all patient group. Over 77% of patients with dementia are living with at least one further health condition, while 22% are living with at least 3 further conditions. Patients with dementia are nearly twice as likely to have 3 or more other specific health conditions and 4 times more likely to have 5 other specific health conditions than the all patient group.
The study found that the proportion of patients with multiple health conditions increases with age for patients with dementia under the age of 85 years. Beyond this age, the proportions with 2 or more comorbidities decreases. These findings may support the view that comorbid condition diagnosis is more difficult to achieve as severity of dementia increases, in particular when age is a proxy for increased severity. This may lead to the underdiagnoses of some conditions that patients with dementia live with [footnote 14].
In addition to the comorbidities analysed in this study, the patients included in the dementia group are also living with dementia. Therefore, in comparing the actual number of health conditions that each group has, it can be said that 100% of patients in the dementia group have at least one health condition, while in the all patient group this proportion is 69%. Furthermore, when including dementia, 8% of patients with dementia have a diagnosis for 5 or more conditions, over 11 times greater than the all patient group (0.7%).
The conclusion that can be drawn from this study is that patients with dementia are more likely to have multiple health conditions when compared to the all patient group. The complexity of the support needed by the individual is increased further when the dementia diagnosis itself is included as part of the health care need.
6.3 Dementia subtypes and comorbidities
The type of dementia that a patient has does influence the comorbidities they also have diagnoses for. Hypertension is a prominent condition with all types of dementia. Three patterns of comorbidities are evident from the THIN dataset. The first group being the dementia types that are Alzheimer’s disease, mixed dementias and unspecified dementia, characterised with 15% to 20% of patients having a diagnosis of diabetes, depression or CHD.
The second group relates to dementia in other diseases and other degenerative diseases of the nervous system. This group is characterised by a high prevalence of Parkinsonism (above 40%) in addition to the high prevalence of hypertension.
The third group is vascular dementia. This type of dementia has a unique pattern of comorbidities with high prevalence rates in excess of 25% for the cardiovascular conditions of stroke/TIA, diabetes and CHD. Hypertension is diagnosed in more than half of patients. Research from Prince [footnote 12] found that male patients are one third more likely to have a diagnosis for vascular dementia than female patients (20% versus 15%). This is reflected in the findings of the study that the largest disparity in prevalence rates for comorbidities between male patients and female patients are for CHD, diabetes and stroke/TIA. Patients with vascular dementia are also most likely to have a diagnosis of COPD (13%) and asthma (9%) than those of other dementia types.
In conclusion, the differing types of dementia do lead to different patterns of comorbidities being diagnosed. Not surprisingly vascular dementia is associated with the cardiovascular conditions, but surprisingly also more associated with respiratory conditions than the other forms of dementia.
6.4 Validation of the findings from THIN dataset
It is not easily possible to validate the findings of this study in terms of the prevalence rates of comorbidities in patients with dementia. However, it is possible to benchmark the calculated prevalence rates for the individual comorbid conditions from the THIN all patient group with the Quality Outcomes Framework.
The findings of the activity suggest that for the conditions of interest in this study, the calculated rates from the THIN dataset are either comparable with the QOF data or have known reasons for the variation. Therefore, it can be assumed that the analysis for the dementia cohort is reasonably reliable given the data collection caveats around the accurate recording of patient health conditions in primary care health systems.
6.5 Considerations for Health and Care Commissioners and Service Providers
Based on the data in this briefing, 77% of people living with dementia also live with other health conditions. These include conditions which are linked to an increased risk of dementia as well as others which have a known association with dementia, including heart disease, stroke/TIA, and diabetes. The NHS Health Check can detect early signs of these conditions and also can reduce the risk of these conditions developing for those aged 40 to 74 years of age.
People living with dementia are more likely to have complex health needs. They are nearly twice as likely to have 3 or more other specific health conditions and 4 times more likely to have 5 other specific health conditions than the all patient group. In determining how to effectively meet the needs of those with multiple and complex health conditions consideration of the specific needs of people living with dementia is appropriate.
The findings of this study may support the view that comorbid condition diagnosis is more difficult to achieve as severity of dementia increases, in particular when age is a proxy for increased severity. This may lead to the underdiagnoses of some conditions that people living with dementia experience. Commissioners and health and care providers may wish to consider the mechanisms they have in place to diagnose, manage and treat the comorbid conditions that people living with dementia experience, particularly those living with more severe dementia.
7. Acknowledgements
The authors of this briefing are various members of the neurology and dementia intelligence team at PHE David Leese, Michael Jackson, Marta Szczepaniak, Julia Verne and supported by Sue Foster, Simran Sandhu.
THIN is a registered trademark of Cegedim SA in the United Kingdom and other countries. Reference made to the THIN database is intended to be descriptive of the data asset licensed by IQVIA.
For more information, please contact MHDNIN@phe.gov.uk
SRC reference number: 17THIN041 THIN is a registered trademark of Cegedim SA in the United Kingdom and other countries. Reference made to the THIN database is intended to be descriptive of the data asset licensed by IQVIA.
8. References
-
Wittenberg. Projections of Older People with Dementia and Costs of Dementia Care in the United Kingdom 2019-2040; Care Policy and Evaluation Centre at London School of Economics and Political Science 2019. Page 7 (viewed November 2019) ↩
-
All Party Parliamentary Group on Dementia. Dementia rarely travels alone: living with dementia and other conditions 2016 (viewed August 2019) ↩ ↩2
-
Vision. The Health Improvement Network (THIN) (viewed August 2019) ↩ ↩2
-
World Health Organisation. International Statistical Classification of Diseases and Related Health Problems 10th Revision 2015 (viewed August 2019) ↩
-
World Health Organisation. International Statistical Classification of Diseases and Related Health Problems 10th Revision 2015 (viewed August 2019) ↩ ↩2
-
NHS Digital. Technology Reference data Update Distribution (viewed August 2019) ↩
-
Madhusoodanan S. Managing psychosis in patients with Alzheimer disease Psychiatric Times 2014 volume 31 (viewed August 2019) ↩
-
NHS Digital. Quality and Outcomes Framework (QOF), enhanced services and core contract extraction specifications (business rules) version 34 (viewed March 2017) ↩
-
Public Health England Neurology Intelligence Network. Defining adult neurological conditions 2016 (viewed August 2019) ↩
-
NHS Digital. Quality and Outcomes Framework, Achievement, prevalence and exceptions data (viewed August 2019) ↩ ↩2 ↩3
-
Prince, M. and others: Dementia UK: Update. Alzheimer’s Society. Page 35 (viewed August 2019) ↩ ↩2 ↩3
-
APHO. Technical Briefing 3: Commonly used public health statistics and their confidence intervals 2008 (viewed August 2019) ↩
-
Scrutton JB. Dementia and comorbidities: ensuring parity of care. International Longevity Centre UK 2016 (viewed August 2019) ↩
