Mindfulness is our human ability to be fully aware of the present moment experience.Reference Siegel, Germer and Olendzki1 In the fast-paced modern world, mindfulness can be difficult to achieve, with many people defaulting to a state of mindlessness.Reference Siegel, Germer and Olendzki1 Mindfulness has gathered momentum in clinical practice, with a growing body of evidence for its application in psychotherapy, pain management and psychiatric disorders.Reference Hofmann and Gomez2,Reference Gotink, Chu, Busschbach, Benson, Fricchione and Hunink3 The positive impact of mindfulness on changing eating behaviours in obese populations attending specialist weight management clinics is established.Reference Hanson, Shuttlewood, Halder, Shah, Lam and Menon4,Reference Felske, Williamson, Rash, Telfer, Toivonen and Campbell5
Obesity and mental health
Obesity is at the forefront of contemporary public health challenges. In 2016, The World Health Organization estimated that 13% of the worldwide population were obese, equating to over 650 million adults.6 In the UK, 27% of men and 30% of women live with obesity.7 Rates of obesity further increased during the current COVID-19 pandemic, with the monthly rate of body mass index (BMI) increase during the pandemic being 1.93 times that of the pre-pandemic rate.Reference Dyer8 This is most likely related to less healthy behaviours, such as unhealthy snacking and reduced activity.Reference Robinson, Boyland, Chisholm, Harrold, Maloney and Marty9
Obesity is very closely associated with mental health issues and stress. Evidence showed that people living with obesity had a 30–70% risk of developing mental health issue over their lifetime.Reference Hert, Correll, Bobes, Cetkovich-Bakmas, Cohen and Asai10 Separate to obesity links to mental health problems, 80% of patients diagnosed with schizophrenia, bipolar disorder or depression were found to be overweight or obese, highlighting a greatly increased prevalence compared with the general population.Reference Correll, Druss, Lombardo, O'Gorman, Harnett and Sanders11 A similar bi-directional association between mental health issues and obesity was found in other large studies.Reference Amiri and Behnezhad12–Reference Luppino, de Wit, Bouvy, Stijnen, Cuijpers and Penninx14 The association of stress with unhealthy eating habits, as well as severe obesity, has been clearly documented.Reference Richardson, Arsenault, Cates and Muth15
In the UK, people with a BMI >40 kg/m2 or >35 kg/m2 with a medical condition such as diabetes can be referred to a specialist weight management service (also called tier 3). Despite increasing referral rates, non-attendance is a significant problem for weight management services, with 28.1% patients found to attend <50% of their follow-up appointments and 17.1% not attending their initial appointments.Reference Brook, Cohen, Hakendorf, Wittert and Thompson16 Mental health factors can play a role in missing appointments, as patients with perceived greater emotional impact of their condition were less likely to attend clinical appointments.Reference Eades and Alexander17
CALMPOD
CALMPOD (Compassionate Approach to Living Mindfully for Prevention of Disease) is an evidence-based group educational course established on principles of mindfulness, such as mindful eating and self-compassion, that has been shown to be feasible in the short term (6 months) and has a positive impact, both in terms of improving eating behaviour and weight loss.Reference Hanson, Shuttlewood, Halder, Shah, Lam and Menon4 CALMPOD is not based on any specific mindfulness programme, such as mindfulness-based stress reduction or mindfulness-based cognitive therapy. It aims to introduce the concept of mindfulness in relation to weight management by exploring mindful eating habits and how mindfulness practice might help to build self-compassion and cope with distress.
The aim of this study was to explore the long-term feasibility of CALMPOD by assessing its impact on patient engagement with the service, weight and metabolic markers.
Method
Intervention
CALMPOD incorporates mindfulness techniques, and its detailed description is available in a previous publication.Reference Hanson, Shuttlewood, Halder, Shah, Lam and Menon4 It comprises four group sessions lasting 90 min each, and is delivered every 2 weeks over an 8-week period. There are between six and 12 participants in each group. The sessions are delivered by a specialised weight management psychologist and specialist weight management dietitian. The topics for the course are mindful eating, introduction to compassionate mind therapy, biological drivers for weight regain, environmental challenges, and development of mindful and compassionate planning and management for relapse.
Study design and participants
This was a retrospective data analysis study based in the clinical context of a specialised weight management service (also called tier 3 weight management service) at University Hospitals Coventry and Warwickshire (UHCW) NHS Trust in the UK. The study was conducted with anonymous clinical data collected between 2016 and 2020. All participants were aged >18 years and had a BMI > 35 kg/m2. The STROBE guidance was used to report the study (Supplementary File 1 available at https://doi.org/10.1192/bjo.2022.602). All referrals across the 4-year period were offered CALMPOD at onset. Because of the COVID-19 pandemic, all face-to-face activity ceased in March 2020; however, data collection for those who attended CALMPOD at an earlier date continued until October 2020. Data on clinic attendance was taken from the hospital administration system. Six-monthly recorded data of all patients were extracted from clinical records for the duration of 24 months from the time of each person's prior course attendance offer. Data collected included regularity of attendance, weight, haemoglobin A1c (HbA1c) and total cholesterol. Data of those patients who had not wished to attend CALMPOD or who dropped out after the first two sessions was compared with those who attended at least three of the four sessions.
Ethics
This was a retrospective, data-driven exercise using routinely collected clinical data by clinicians of the team. The project used anonymised pooled data from the centre. No individual patient data was shared outside the direct clinical team (lead author and last author). This work has been approved by Research and Development Department at UHCW and did not need any formal ethical approvals. Data were collected as part of an ongoing service evaluation and registered as such in the organisation; data were collected retrospectively from existing clinical records. We also used the NHS Health Research Authority tool (http://www.hra-decisiontools.org.uk/research/index.html), which confirmed no formal NHS ethical approval was required (Supplementary File 2). No non-organisation author had access to any patient-identifiable information. All patients provided verbal consent to take part in the group educational course, which was part of weight management service.
Statistical analysis
The χ²-test was used for analysis of appointment attendance. Independent student test or χ²-test was used to compare baseline characteristics between two groups. To account for the correlation between repeated observations made on participants’ weights, a linear mixed-effects (repeated measures) regression model was used to quantify and draw inferences on the participant data.
Analysis of the weight data was performed with linear mixed models, to allow for the repeat measurements from the same patients over time. An autoregressive correlation structure was used to allow for the order of the measurements over time.
To calculate the rate of change in each group, time was first considered as a continuous variable. The interaction between time and group was included to compare the rate of change in the two groups. Second, time was considered in categories, to quantify the group difference at each time point. For these analyses, the baseline (time 0) values were excluded from the analysis, with the baseline weight included as a covariate in the model. The interaction between group and time was included to obtain the separate effect at each time point.
Results
Baseline characteristics
There were 163 patients who attended at least three of the four CALMPOD course sessions and 126 patients who did not, and whose data was used to compare with the participants. The mean baseline weight was 133.1 kg for the CALMPOD group and 137.1 kg for the comparison group. Nearly 75% of patients in both groups were women, and the mean HbA1c for both groups was at a pre-diabetes level of around 45 mmol/mol. A quarter of patients had diabetes in the CALMPOD and comparison groups (24.4% and 26%, respectively). There was no baseline difference of note in these characteristics between the groups (shown in Table 1).
Table 1 Baseline characteristics

CALMPOD, Compassionate Approach to Living Mindfully for Prevention of Disease.
Patient engagement with the service
There was a marked difference between CALMPOD and comparison groups in follow-up attendance. The CALMPOD group was much more likely to engage with the service and attend regular appointments, with 99% (161 out of 173) attending their 6-month follow-up and 56% (92 out of 163) attending their 2-year follow-up; this was significantly more than the 73% (92 out of 126) and 40% (51 out of 126) attendance in the control group. χ²-Test analysis showed that the difference between groups was significant at all four time points, with P values of <0.001, <0.001, 0.004 and 0.007 for months 6, 12, 18 and 24, respectively. Visual representation can be found in Figure 1. However, when the trajectories of attendance rate over 24 months between the two groups were compared including terms for time and group, along with the interaction between these two terms in the mixed model, no statistical difference between groups in terms of changes over time was identified (P = 0.63).

Fig. 1 Follow-up attendance.
Changes between groups
There was no statistically significant difference between the groups in terms of starting weight, age, baseline HbA1c and lipid levels. Mean weight loss was 5.6 kg (s.d. 11.2) and 3.9 kg (s.d. 10.5) at 24 months for the CALMPOD and comparison groups, respectively, with an absolute difference of 1.7 kg between the two groups. There was a statistically significant weight loss over time in both group participants. However, the rate of weight loss was not statistically different between the CALMPOD and comparison groups (P = 0.939). The mixed-model analysis showed that the gradient of weight loss over time was 0.22 kg per month (P <0.001) in the CALMPOD group and 0.17 kg per month (P ≤ 0.001) in the comparison group. Based on the mixed-model analysis, the calculated difference in weight loss between the groups was 1.2 kg at 24 months. Weight changes over time are shown in Figure 2.

Fig. 2 Weight changes over time, with bars representing s.e. of the mean.
To calculate the rate of change in weight over time, time was included as a continuous variable in the regression model. The non-linearity of the time effects was investigated by including higher-order terms for time (quadratic and cubic terms). These did not improve the fit of the regression model. This finding, along with visual plots of the data, suggested no evidence that there was a non-linear relationship between weight and time. The second model of using time in categories was also explored, and there were no significant results to report (Table 2).
Table 2 Weight changes over time
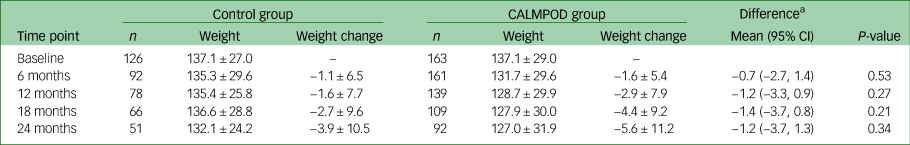
Summary statistics are presented as mean ± s.d. CALMPOD, Compassionate Approach to Living Mindfully for Prevention of Disease.
a. Difference reported as weight in the CALMPOD group minus weight in the control group. Differences adjusted for weight at baseline.
The reduction in HbA1c was 0.91 mmol/mol and 0.01 mmol/mol in the CALMPOD and control groups, respectively; however, the difference was not statistically significant. Similarly, there was not a significant difference in total cholesterol change between the groups, with 0.22 mmol/L and 0.18 mmol/L reduction in the CALMPOD and control groups, respectively.
Discussion
This is, to our knowledge, the first study investigating the long-term impact of mindfulness-led eating and compassion-based techniques incorporated into a group education course among patients attending a specialised obesity service. We found that a mindfulness and compassion-based course is associated with improvements in long-term clinical follow-up rates and leads to a significant weight loss over time. It is worth highlighting that there was significant weight loss over time in the control group as well.
A growing evidence base exists to support the use of mindfulness and compassion-based techniques in clinical practice. A recent meta-analysis of 21 randomised controlled trials of third-wave cognitive–behavioural therapies that use mindfulness concepts, such as mindfulness-based cognitive therapy and compassion-focused therapy, found that the intervention contributed to greater weight loss than standard behavioural treatment.Reference Lawlor, Islam and Bates18 This analysis found that the weight loss difference was 0.6 kg immediately post-intervention and 1.4 kg at the 24-month follow-up.Reference Lawlor, Islam and Bates18 This is similar to our study findings of 0.7 kg at 6 months and 1.7 kg at 24 months. The evidence supports incorporation of mindfulness techniques into clinical practice, both for improvements in patient engagement with the service and long-term weight outcomes.
The mean weight in the control group at month 18 was higher than at months 6 and 12, but the percentage weight change and changes in weight at month 18 was much lower than at months 6 and 12 (Fig. 2). The reason for this is the different numbers of participants in the analysis at the different time points. For example, there were 78 participants in the control group with data at 12 months, but only 66 at 18 months. In the control group, the baseline weight of patients with data at 12 months was 137.0 kg, but at 18 months it was 139.3 kg. Thus, because of the different baseline values within these two subgroups, the actual weight at 18 months was higher than at 12 months, but the reduction in weight was greater.
Limitations of the study
Limitations of this study include its observational nature, small sample size, lack of psychological assessments and its design as a single site study. Given its nature as a retrospective observational study, confounding and bias effects, such as changes to patients’ medications, education, social status self-selection and motivation, would have played role. It could be argued that there was participant bias as those more motivated to lose weight were more engaged with the course. However, this project was an explorative study to identify suitable associations for further inquiry, and not causality. Further, the same clinicians delivered the care in the control group, and were therefore likely to be offering the same advice and support as in the group, on an individual level. However, patients attending the CALMPOD group had more interactions with the clinical team, which could have fostered more motivation and contributed to improved attendance rates. We did not measure changes in mindfulness level and long-term eating behaviour changes, nor was an inquiry made into baseline psychological levels, socioeconomic status or education levels.
Finally, it is not clear to what extent the results were confounded by the effect of the global COVID-19 pandemic. However, as most of the data collection occurred pre-pandemic, it is likely that only a small proportion of the data were directly affected by the pandemic. Nevertheless, it is clear that the pandemic contributed to worsening obesity rates, and the impact of this will continue to be observed in years to come.
Implications for clinical practice
The mainstay of obesity management is lifestyle changes, including increasing physical activity and reducing caloric input.19 Albeit effective in the short term, the evidence of sustained weight loss following these interventions is poor, with over a third of weight being regained within the first year.Reference Maclean, Bergouignan, Cornier and Jackman20 The challenge for the individual who is aiming to sustain weight loss is in complying with behaviours that counteract their own physiology.Reference Greenway21 The onus should be on clinicians to provide their patients with the tools to develop effective and sustainable behavioural modifications that go further than instructions to simply reduce calorific intake. Obesity management should be focused on preparing the patient mentally for the challenges of a healthy lifestyle change. The fact that patients engaged better with the service after the CALMPOD intervention is an important outcome for both patient and health services.
Implications for research
In this retrospective, data-driven observational study, we assessed 24-month outcomes of the mindfulness-based educational course CALMPOD in a clinical setting of a specialised weight management service. The results of this study suggest a positive association of such a course on patient engagement, as well as significant weight loss over time, with little resource expenditure. To provide robust evidence on the effectiveness of such interventions, multi-site randomised controlled trials need to be set up. Additionally, measures of mindfulness scores and validated questionnaires on eating behaviours and psychological health (e.g. depression, anxiety) should be collected. To further explore factors predictive of non-attendance, variables such as educational level, marital status and socioeconomic status should be collected, as they have been shown to affect rates of non-attendance in previous studies.Reference Wolff, Waldorff, von Plessen, Mogensen, Sørensen and Houlind22
Supplementary material
Supplementary material is available online at http://dx.doi.org/10.1192/bjo.2022.602
Data availability
Anonymised data that support the findings of this study are available from the corresponding author, R.S., upon reasonable request.
Author contributions
Conceptualisation: P.H., E.S., T.M.B., V.M., H.S.R. Methodology: P.H., M.L., T.M.B. Formal analysis and investigation: E.S., D.O.-D., M.L., T.M.B., R.S. Writing – original draft preparation: P.H., M.L., D.O.-D. Writing – review and editing: R.S., R.T.A., M.O.W., T.M.B. Supervision: R.T.A., R.S., T.M.B., M.O.W., V.M., H.S.R.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
R.S. and R.A. are members of the Editorial Board for BJPsych Open and did not have any involvement in the review process.
R.S. has received institutional and research support from LivaNova, Union Chimique Belge (UCB), Eisai, Special Products, Bial, GW/Jazz Pharma, Angelini Pharma and Desitin, outside the submitted work. R.S. is a panel member of the National Institute for Health and Care Excellence committee for the update of the guidance for epilepsy and is the medical lead of the Sudden Unexpected Death in Epilepsy (SUDEP) and Seizure Checklist/EpSMon project. R.S. is the principal or co-applicant of various grants, including from NHS England, National Institute for Health and Care Research, Economic and Social Research Council (ESRC), Engineering and Physical Sciences Research Council, Bailey Thomas Fund and Small Business Research Intiative, all outside the submitted work. P.H. received grants from Health Education England and AstraZeneca, outside the submitted work. The other authors have no conflicts of interest to declare.










eLetters
No eLetters have been published for this article.